OVERVIEW OF OBESITY
The World Health Organization (WHO), along with numerous national and international medical and scientific organizations, now classifies obesity as a chronic, progressive disease driven by a combination of environmental and genetic factors. It is no longer viewed as merely a cosmetic problem caused by overeating or a lack of self-discipline. Obesity affects people of all ages, races and socioeconomic backgrounds.

DEFINITION OF OBESITY
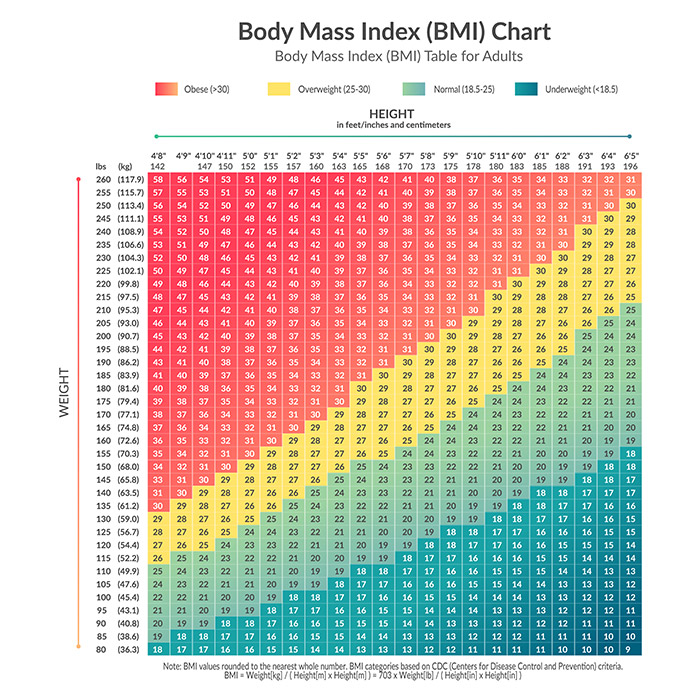
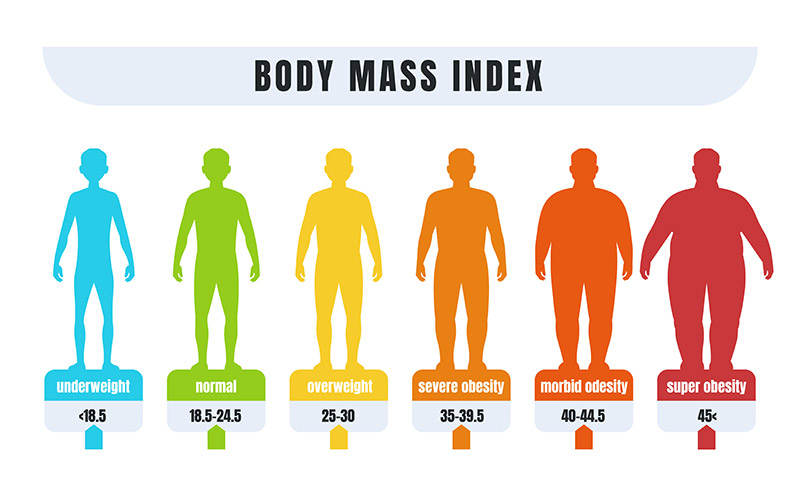
Obesity is defined using the Body Mass Index (BMI) as a measure of body fat based on a person’s weight and height. According to the World Health Organization (WHO), obesity is typically categorized as follows:
- Normal weight: BMI between 18.5 and 24.9
- Overweight: BMI between 25 and 29.9
- Obesity: BMI of 30 or greater
CAUSES OF OBESITY
Obesity is a multifaceted condition with various contributing factors. It occurs when the body stores excess calories as fat.
1. Genetics: Certain genes are linked to obesity and being overweight, it also impacts lifestyle choices.
2. Eating Habit: Consuming more calories than your body requires, along with eating ultra-processed foods, sugary foods and drinks, and items high in saturated fats, can contribute to weight gain.
3. Physical activities: A lack of physical activity is another key factor contributing to obesity, due to excess energy gained from consumption of food and inadequate exercise. This excessive energy gets stored as fat.
4. Underlying health issues: Conditions such as metabolic syndrome, hypothyroidism, and polycystic ovary syndrome can lead to side effects like weight gain. Mental health challenges, including anxiety and depression, may result in cravings for high-calorie foods that trigger the brain’s pleasure centers.
5. Medications: Some medications, including steroids, drugs used to treat epilepsy and diabetes, as well as certain medications for mental health conditions—such as antidepressants and antipsychotics for schizophrenia—can contribute to weight gain.
6. Stress: When you are stressed or lack of sleep, your brain and body produce more hormones, such as cortisol, that affect hunger. This often leads to cravings for high-fat, high-sugar comfort foods, which your body tends to store as additional fat.
OBESITY RELATED MEDICAL CONDITIONS
- Cardiovascular diseases (hypertension, stroke, heart failure, heart attack)
- Respiratory distress (obstructive sleep apnea)
- Endocrine disorder (diabetes, thyroid dysfunction, polycystic ovarian syndrome, infertility, sexual disfunction)
- Cancer
- Fatty liver disease
- Kidney disease
- Gallstones
- Acid reflux
- Arthritis
- Depression/anxiety

TREATMENTS
Current medical management for obesity typically involves a combination of lifestyle changes, medications, and sometimes surgery, depending on the severity of obesity and individual health conditions. Here’s a brief overview:
1. Lifestyle Modifications:
- Diet: A calorie-reduced, balanced diet that emphasizes whole foods, lean proteins, and healthy fats.
- Exercise: Regular physical activity (at least 150 minutes per week) to promote weight loss and improve overall health.
- Behavioral Therapy: Cognitive behavioral strategies to help individuals manage emotional eating, cravings, and develop sustainable habits.
2. Medications
Prescription weight-loss medications may be used when lifestyle changes alone are not enough. These can include:
- Orlistat: Reduces fat absorption in the intestines.
- Phentermine-topiramate (Qsymia): An appetite suppressant and stimulant combination.
- Liraglutide (Saxenda): Mimics a hormone that helps control hunger.
- Semaglutide (Wegovy): A GLP-1 receptor agonist that helps control appetite and food intake.
3. Surgical Options
For individuals with severe obesity (BMI > 40 or > 35 with comorbidities), bariatric surgery may be considered. Common procedures include:
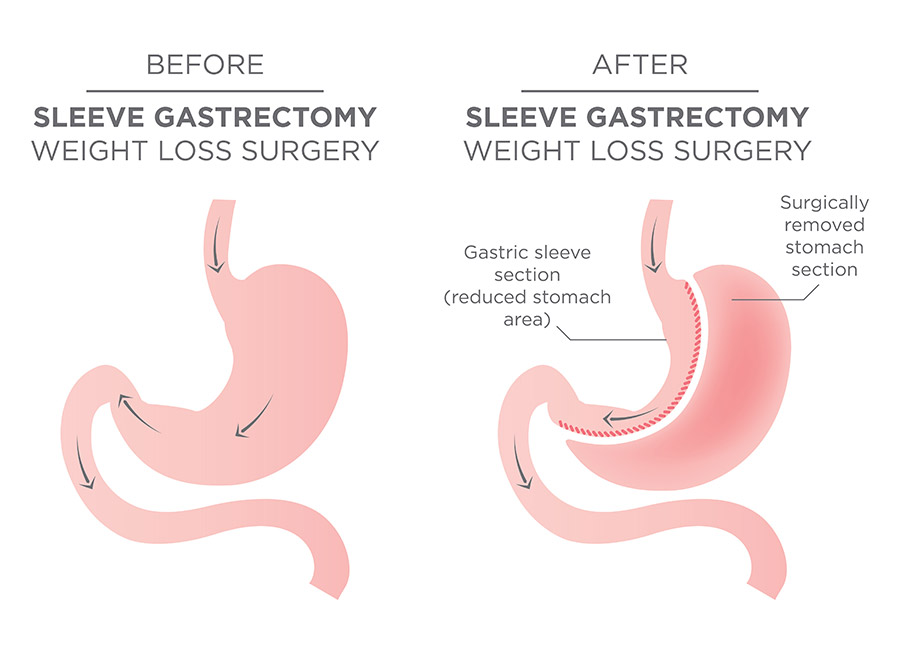
- Sleeve Gastrectomy: Removes a large portion of the stomach, reducing its size and limiting hunger.
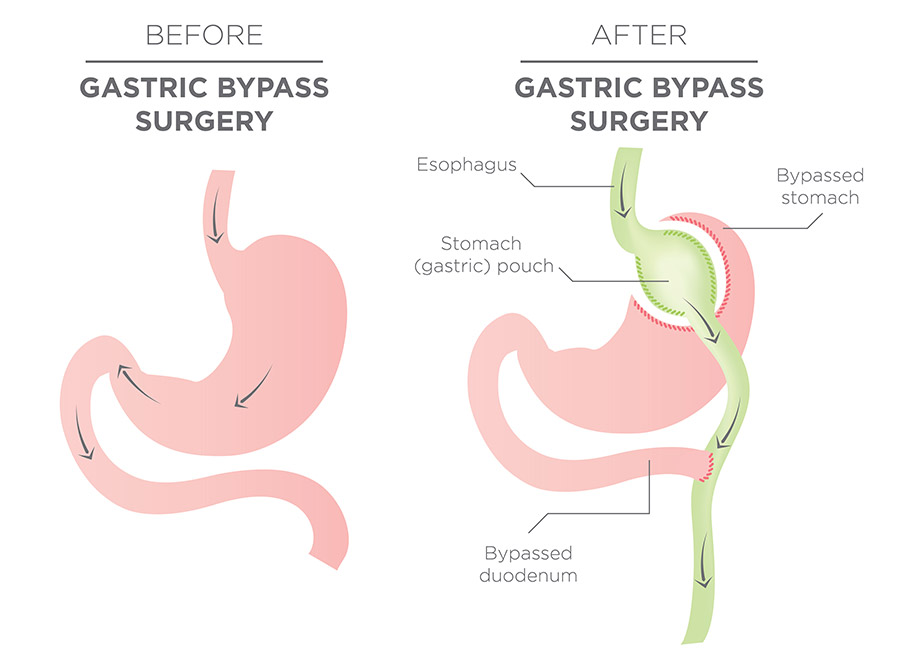
- Gastric Bypass: Reduces the size of the stomach and bypasses part of the intestine, limiting food intake and nutrient absorption.
- Adjustable Gastric Banding: Involves placing a band around the stomach to limit food intake, although this procedure is not commonly performed anymore.
- Revisional Surgery: This is indicated if an individual who had a prior weight loss surgery and has gained weight or developed complications.
Qualifications for surgery
**Based on the ASMBS guideline in 2022:**
BMI > 30 with obesity-related medical conditions
Or BMI > 35 alone with or without medical problems
However, some insurances still follow the old guideline, which was > 35 with medical problems or BMI > 40